Dec 06, 2017
Graduate Nurse Education: A Pathway to Increased Primary Care Access
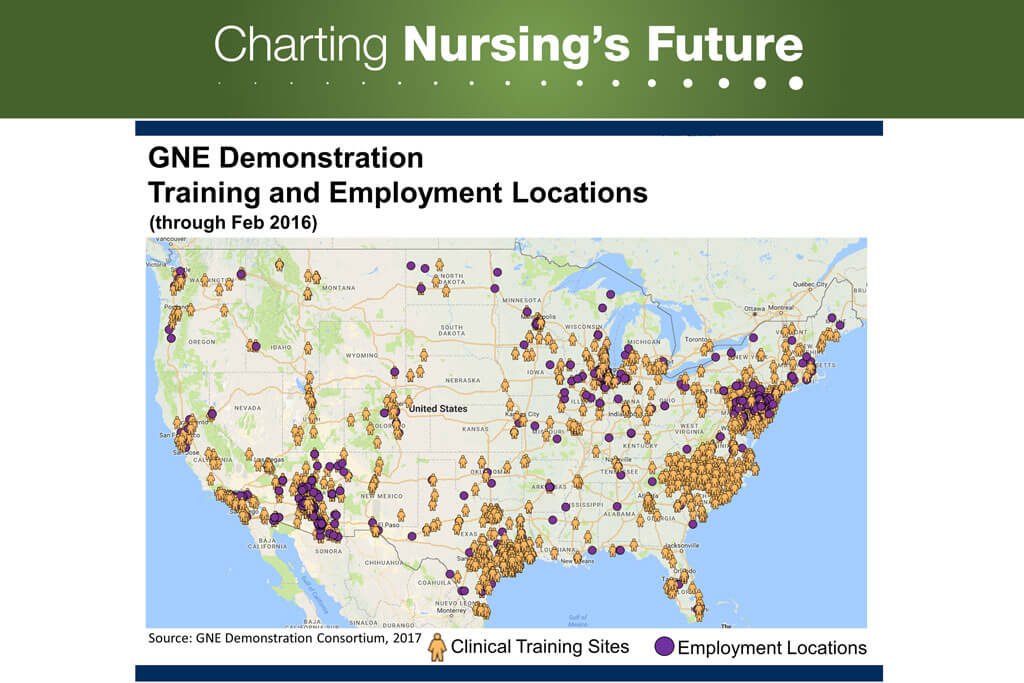
Medicare Graduate Nurse Education dollars were directed at five demonstration sites, but the Medicare clinical training dollars reached all 50 states and three territories. As of 2016, 7,864 APRN students were educated through this program, and were employed in 46 states. Courtesy of Linda H. Aiken, University of Pennsylvania, for the GNE Demonstration Consortium.
What if—in just a matter of years—nurses found a way to solve a problem that has been brewing for decades?
Findings from the Graduate Nurse Education (GNE) Demonstration Project suggest nursing has uncovered a promising avenue for increasing the number of primary care providers at a time of national shortage. According to Linda Aiken, RN, PhD, who spearheaded the effort at the University of Pennsylvania (Penn), one of five GNE demonstration sites, “APRNs could vastly improve access to primary care if we had enough of them. We demonstrated we can close the gap if we just have funding.”
But let’s back up. Exactly what did the GNE Demonstration Project set out to do, and why?
The project tested, for the first time, whether it is feasible and productive to use Medicare funding to support clinical training for advanced practice registered nurses (APRNs) and to shift some training from hospitals to community-based settings. Medicare has been funding the clinical training of physicians through hospital-based residency programs for decades.
Enabling nursing schools to enroll and graduate more APRNs served several objectives: increasing access to chronic care management, pain management, and women’s health care among them. The project also aimed to increase access to primary care by graduating more nurse practitioners (NPs), many of whom would be prepared to deliver primary care in community-based settings. To achieve this goal, planners made it a priority to situate the newly funded clinical training opportunities in community health centers and retail clinics.

Linda Aiken, RN, PhD, is a professor of nursing at the University of Pennsylvania and a vocal proponent of federal funding for Graduate Nursing Education.
During the demonstration, enrollment and graduation rates for NPs increased far more at GNE than at non-GNE schools of nursing. Even more impressive, 70 percent of clinical training placements by the GNE schools occurred in community settings rather than hospitals, with researchers documenting a steady shift in NP clinical-education hours from hospitals to the community.
How did organizers manage to place so many students in community settings? Aiken, who is a professor of nursing and director of the Center for Health Outcomes and Policy Research at Penn, credits “feet on the ground.” It’s easier to train health care professionals in hospitals, she explains, because there are so many people around who might serve as preceptors (on-the-job instructors). To identify alternative practice sites, organizers approached primary care providers one-by-one to present both the benefits of taking on a graduate student and the project’s ability to offset some of the costs.
Supervising a student will inevitably impinge on a provider’s time, making it difficult to see a patient every 15 minutes, as many practices expect. GNE funding helps compensate clinical sites for this loss of productivity, enabling their providers to act as preceptors. “This is why the funding is so important,” Aiken says.
Another exciting discovery of the demonstration project: It established that hospitals can be recruited to receive and manage Medicare funds earmarked for use in the community. “This is a tremendous finding,” says Aiken. In the GNE model, each hospital works as a hub at the center of a “geographic consortium” made up of the hospital, area nursing schools, and community health care providers, all striving to bring students together with clinical training sites, preceptors, and the oversight apparatus needed to manage it all.
The demonstration project showed that onsite clinical training to prepare an APRN to practice primary care costs about $30,000 per student. That’s a bargain when compared to the roughly $150,000 it costs per year to fund clinical residency training to prepare a single primary care physician through another community-based Medicare demonstration project.
Of course, no matter how inexpensive, the program cannot continue beyond June 2018 without additional approved funding. (GNE was originally funded from 2012 to 2016 and was subsequently extended to 2018 with unused funds from the original grant.) Advocates including Aiken have been working for years to develop a plan for a permanent and national solution that would include Medicare support for clinical training of all APRNs. In the interim, advocates hope to advance legislation that would provide an additional $80 million to extend funding for the five current demonstration project sites through 2020.
The effort is not without some urgency. “We have a national shortage of primary care providers that has been in the works for over four decades,” explains Aiken. “With fewer and fewer U.S. physicians choosing primary care as a career, the increased training and graduation of APRNs who practice primary care offers a viable solution that we shouldn’t ignore.”
